Bone Marrow Transplants
Bone marrow transplants are transformative treatments designed to replace damaged or diseased bone marrow with healthy cells. These transplants restore the body’s ability to produce healthy blood cells, offering new hope to patients with severe blood disorders, compromised immune systems, and certain cancers.
The Science Behind Bone Marrow Transplant
Bone marrow plays a critical role in producing red blood cells, white blood cells, and platelets. When disease, chemotherapy, or other factors damage the bone marrow, a transplant introduces healthy stem cells into the bloodstream to regenerate functional marrow.
These transplants can be performed using stem cells from a donor (allogeneic transplantation) or the patient’s own stem cells (autologous transplantation), depending on the condition being treated. Advancements in Human Leukocyte Antigen (HLA) matching have significantly reduced complications like graft-versus-host disease, making the procedure safer and more effective than ever.
Key Benefits of Bone Marrow Transplants
Restores Healthy Blood Cell Production
Enables the body to produce red cells, white cells, and platelets essential for survival.
Strengthens the Immune System
Helps rebuild immunity compromised by disease or intensive treatments like chemotherapy.
Treats Genetic Blood Disorders
Addresses various genetic blood disorders like Sickle Cell disease by replacing the underlying defective bone marrow.
Effective for Severe Blood Disorders
Treats hereditary and acquired blood conditions like sickle cell disease and aplastic anemia.

Why Choose JCRC-ABT CellGene Innovations?
At JCRC-ABT CellGene Innovations, we combine modern science with compassionate care to deliver life-saving bone marrow transplants. From donor matching to post-transplant recovery, we are committed to providing exceptional support at every step.
1. What conditions can bone marrow transplants treat?
Bone marrow transplants are used to treat blood cancers (e.g., leukemia, lymphoma), severe blood disorders (e.g., sickle cell anemia, aplastic anemia), and immune deficiencies.
2. What is the difference between allogeneic and autologous transplants?
Allogeneic transplants use stem cells from a donor, while autologous transplants use the patient’s own stem cells, typically harvested before intensive treatments.
3. How safe is the procedure?
Bone marrow transplants use proven techniques and are performed under strict medical protocols to minimize risks. Side effects are managed by our experienced team, and long-term survival rates have improved significantly.
4. How is a donor match determined?
Donor compatibility is based on Human Leukocyte Antigen (HLA) matching. Advanced matching techniques at JCRC-ABT reduce complications and improve outcomes.
5. How long is the recovery process?
Recovery times vary by patient. While initial recovery may take a few weeks, full immune system restoration can take several months to a year.
CASE STUDY
Case Studies on Bone Marrow Transplant
Severe Combined Immunodeficiency (SCID)
A study in The Journal of Clinical Immunology showed that haploidentical BMT restored immune function in infants with SCID. T-cell reconstitution was achieved in 85% of cases, with a survival rate of 90% at 2 years, enabling these children to live infection-free with normal immune responses.
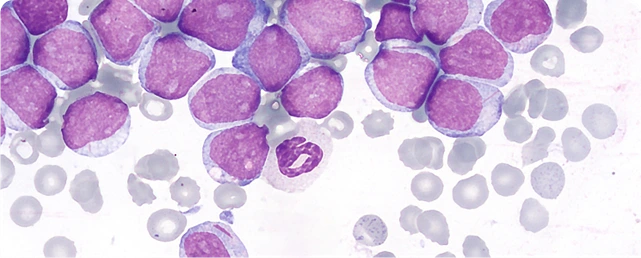
Acute Myeloid Leukemia (AML)
Research in The New England Journal of Medicine demonstrated that BMT significantly improved relapse-free survival in patients with high-risk AML in first remission. Long-term follow-up revealed a 60% overall survival rate at 5 years, compared to 30% for patients receiving only chemotherapy.
Sickle Cell Disease
A study published in Blood Advances highlighted curative outcomes for children with severe sickle cell disease after allogeneic bone marrow transplantation (BMT) from HLA-matched sibling donors. Over 90% of patients achieved stable engraftment and complete resolution of sickle cell-related symptoms, with a 5-year survival rate exceeding 95%.
